
Colonic diverticulitis is a condition commonly affecting individuals consuming a western diet. When the inner layer of colon (large intestine) protrudes through the wall of the colon as a small out pouching, a diverticulum is formed. When multiple diverticula are present, the condition is called diverticulosis. When the diverticula become inflamed or infected, the condition is called diverticulitis. Diverticular disease is a term that includes both diverticulosis and diverticulitis.
Clinical features
 The exact cause of diverticular disease is unknown. Western diet and paucity of fiber is thought to play a central role. Many patients have diverticular disease without symptoms. Other patients may experience signs and symptoms of diverticulitis as a result of inflammation and infection of the diverticula and the surrounding segment of colon. These include abdominal pain, fever, nausea, vomiting, change in bowel habits, bloating, etc. Patients with diverticulosis may experience bleeding. Bleeding is usually in the form of bright red blood per rectum and may be brisk.
The exact cause of diverticular disease is unknown. Western diet and paucity of fiber is thought to play a central role. Many patients have diverticular disease without symptoms. Other patients may experience signs and symptoms of diverticulitis as a result of inflammation and infection of the diverticula and the surrounding segment of colon. These include abdominal pain, fever, nausea, vomiting, change in bowel habits, bloating, etc. Patients with diverticulosis may experience bleeding. Bleeding is usually in the form of bright red blood per rectum and may be brisk.
Complications
Most patients with diverticular disease do not experience complications related to the disease. However those who do are subject to potentially serious complications. These include:
1. Infection in the form of an abscess or a large phlegmon (indistinct mass): Serious infection is usually the result of perforation of an inflamed diverticulum. If body’s own surrounding tissues wall off the perforation, an abscess is formed. This will require admission to the hospital, intravenous antibiotics, and emergency drainage of the abscess by an interventional radiologist. Sometimes, the abscess cannot be drained and patients will require an emergency surgery and temporary colostomy. If body is unable to wall off the perforation, and the infection spread to the entire abdominal cavity, patient will require an emergency surgery and temporary colostomy.
2. Bleeding that may be severe and require hospitalization and blood transfusion: Because blood vessels travel through the diverticula, bleeding from diverticulosis of colon is often brisk and patient may lose significant blood within one or two days. This is an indication for surgery. A temporary colostomy may sometimes be required.
3. Obstruction of colon: As a result of repeated attacks of diverticulitis, colonic lumen may get narrowed to a point where stool may no longer pass easily resulting in obstruction. Colonic obstruction is an indication for urgent or emergent surgery.
Diagnosis and Treatment
Diverticular disease is either detected during a colonoscopy or with a CT scan. If the disease is identified during a routine colonoscopy and patient has not history to suggest prior symptoms, no further treatment is required except a diet rich in fiber and low in residue (nuts and seeds).
However if a patient has had at least two or three attacks of acute diverticulitis surgery is indicated to prevent future attacks or to prevent complications. If a patient presents emergently with any of the complications listed above surgery will be required on an urgent or emergent basis.
Laparoscopic Colectomy
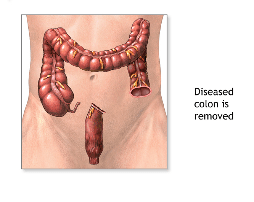
Laparoscopic colectomy is the procedure in which the affected segment of colon is removed surgically using minimally invasive techniques. If the procedure is performed electively when the colon is not inflamed or infected, your surgeon can remove the diseased segment of the bowel and reattaches the unaffected parts together, all in one stage. It is therefore important to seek surgical advice if you meet any of the indications listed above and before the onset of the next attack.
If the surgery has to be performed during an active bout of inflammation or when the overall hemodynamic condition of the patient is unfavorable as a result of systemic infection, a temporary colostomy is usually created. A colostomy is created when the top portion of the colon is brought out through a hole in the abdominal wall into a bag. Patient will then require a second operation after two to three months to reattach the healthy segments. This is called a two-stage approach, which can be avoided in many instances.